|
Case Report
Unusual and rare manifestations after bronchoscopy: Pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum—Case report
1 Department of Radiology, Faculty of Medicine, Mohammed VI University of Sciences and Health – UM6SS, Casablanca, Morocco/Cheikh Khalifa International University Hospital, Casablanca, Morocco
Address correspondence to:
Amrani Chaimae
82 AV Mohamed Taib Naciri, Commune de Casablanca, Casablanca, Settat 20270,
Morocco
Message to Corresponding Author
Article ID: 100132Z06AC2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Chaimae A, Samia B, Rayhana CS, Anass AR, Mahamoud CA, Nour AE, Othman A, Amal R. Unusual and rare manifestations after bronchoscopy: Pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum—Case report. Case Rep Int 2025;14(1):10–15.ABSTRACT
Introduction: Pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum are rare findings in the absence of visceral perforation or trauma. While often asymptomatic, these conditions can complicate clinical decision-making, particularly when they occur after endoscopic procedures such as bronchoscopy. Typically caused by barotrauma, air leakage in such cases is often explained by the Macklin effect—a phenomenon where air dissects through the interstitial tissues following alveolar rupture. Although flexible bronchoscopy is generally considered a safe procedure, timely recognition of these complications is essential to prevent adverse outcomes. Medical imaging, especially computed tomography (CT), plays a vital role in diagnosing these conditions, evaluating associated complications, and identifying potential underlying causes such as perforation.
Case Report: We report the case of a 17-year-old female patient hospitalized for surgical management of a left pulmonary hydatid cyst. Following a diagnostic bronchoscopy, the patient developed pneumomediastinum, pneumoperitoneum, and pneumoretroperitoneum. Imaging studies were instrumental in the rapid identification of these rare complications. Despite radiological findings suggestive of visceral perforation, further endoscopic evaluations revealed no injury to the esophageal, digestive, or bronchial structures. The patient was admitted to the intensive care unit for close monitoring due to an initially unstable clinical condition. The management was conservative, and the patient’s condition improved progressively. He was discharged without any further complications.
Conclusion: This case highlights the importance of imaging in the diagnosis and monitoring of rare complications following bronchoscopy. Even in the absence of overt visceral injury, clinicians should be aware of these potential presentations to ensure prompt and appropriate management.
Keywords: Bronchoscopy complications, Case report, Pneumomediastinum, Pneumoperitoneum, Pneumoretroperitoneum
INTRODUCTION
Bronchoscopy is a widely used diagnostic and therapeutic procedure, generally regarded as safe with a low complication rate. However, like any medical intervention, it involves certain risks, and various adverse events have been documented [1].
While flexible bronchoscopy is typically deemed safe, the concurrent occurrence of pneumomediastinum, pneumoperitoneum, and pneumoretroperitoneum remains extremely rare. In most cases, these conditions resolve on their own with conservative management involving a multidisciplinary approach. However, when trauma is involved, pneumomediastinum can complicate diagnosis as it may resemble other critical conditions, such as esophageal perforation, bowel rupture, or tracheobronchial injuries. This diagnostic ambiguity can result in unnecessary interventions if not correctly identified.
We present the case of a 17-year-old female patient hospitalized for the treatment of a left pulmonary hydatid cyst, who developed pneumomediastinum, pneumoperitoneum, and pneumoretroperitoneum after undergoing a diagnostic bronchoscopy. This case underscores the importance of early recognition of such complications and highlights the crucial role of medical imaging in avoiding unnecessary surgical interventions [2].
CASE REPORT
We report the case of a 17-year-old female patient with no significant medical or surgical history, who was initially admitted for the evaluation of a hydatid cyst in the left lung. She underwent bronchoscopy under sedation, which proceeded without complications until the end of the procedure. Shortly afterward, she developed marked abdominal distension accompanied by diffuse abdominal pain and generalized guarding on clinical examination.
Given the hemodynamic and respiratory instability, the patient was intubated, ventilated, sedated, pupils symmetrically miosis, and stabilized under noradrenaline 0.2 mg/h, blood pressure: 102/65, heart rate (HR): 134 beats/min, respiratory rate: 16 cycles/minute, oxygen saturation 91% under 100% FiO2, pleuro-pulmonary examination objective of snoring and crackling rales at both pulmonary bases.
Correct Diuresis Greater than 1 mL/kg/h, Apyretic
Given the following diagnostic elements, after monitoring, sedation with noradrenaline and surveillance, antibiotic therapy was initiated with double-dose gastric protection.
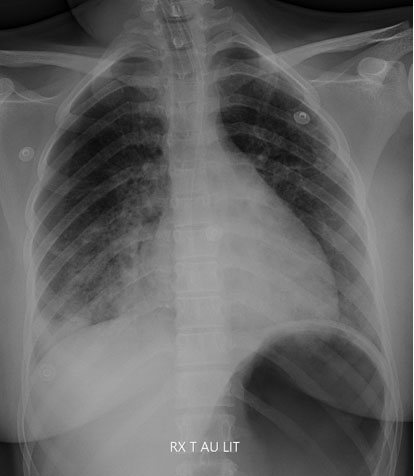
An initial radiological workup was performed with a chest X-ray (Figure 1) where no pneumomediastinum or pneumothorax was found, with visualization of an enlarged thoracic cavity.
Biological workup requested: Hemoglobin 12.2 and platelets 491,000/mm3, C-reactive protein (CRP) 26.5, with a normal renal workup.
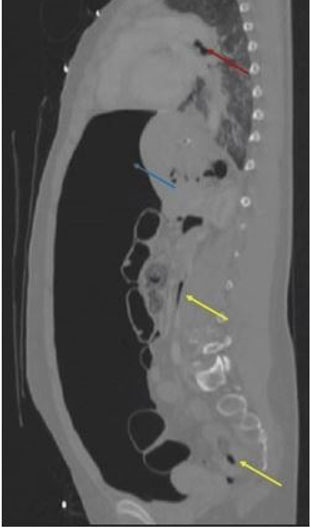
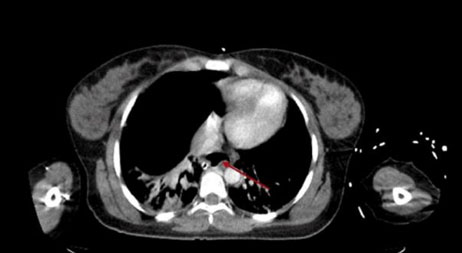
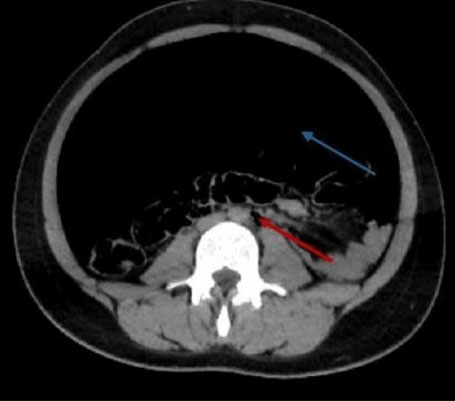
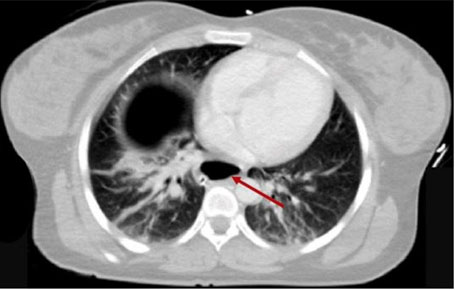
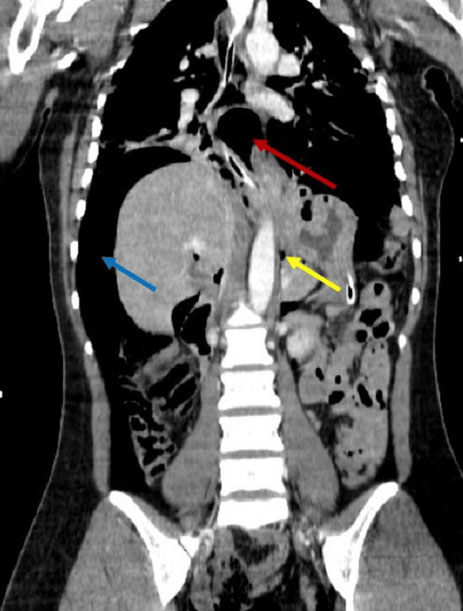
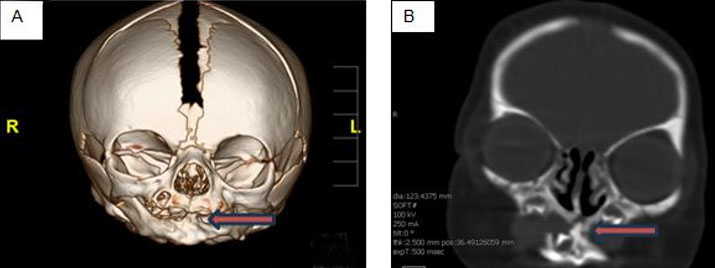
A cervico-thoraco-abdomino-pelvic scan (Figures 2, Figure 3, Figure 4) was performed, revealing pneumomediastinum (Figure 3 and Figure 5), a large pneumoperitoneum and pneumoretroperitoneum (Figure 4). The patient’s condition rapidly deteriorated, becoming hemodynamically unstable with hypotension, diffuse tenderness, altered consciousness, respiratory distress, and the onset of acute pulmonary edema with pinkish, frothy secretions. Due to the severity of her condition, she was urgently moved to intensive care unit, where she underwent intubation and was placed on mechanical ventilation.
Following resuscitation with adequate amounts of noradrenalin and saline, the patient was sedated and maintained an acceptable oxygen saturation level under moderate mechanical ventilation settings, and was vitally stable (blood pressure = 12/60 mmHg; heart rate = 91 bpm), she was stable enough to undergo imaging.
After initial stabilization with protective ventilation. The patient was taken to the operating room for an exploratory laparotomy. However, imaging revealed no evidence of gastric or duodenal perforation, peritoneal effusion, or appendicitis.
Following surgery, she was readmitted to the intensive care unit for ongoing monitoring and treatment. A follow-up bronchoscopy was conducted, showing no abnormalities.
After a 5-day hospitalization, our patient was hemodynamically stable on noradrenaline 3.5 mg/h and dobutamine 5 µg/h. Given the renal management and good clinical evolution over the following two days, the patient was extubated and weaned off noradrenaline with dobutamine, oral re-feeding was initiated without incident.
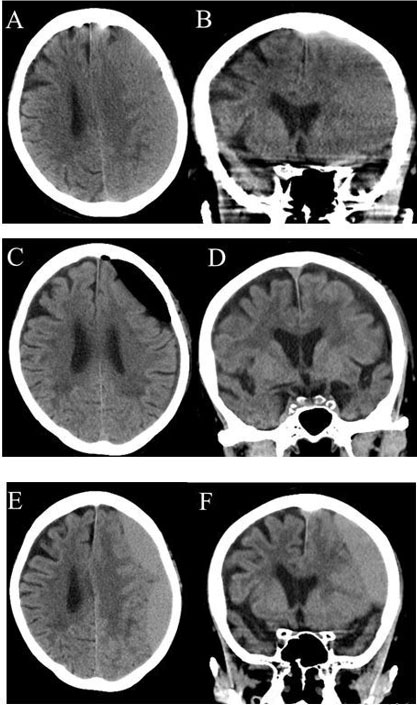
D3 after intubation, the patient was conscious and stable both hemodynamically and in terms of respiratory function (under a small dobutamine fund), with a flexible abdomen. D4 after intubation and dobutamine withdrawal was performed, a control imaging was performed that no longer objectified pneumoperitoneum or retropneumoperitoneum (Figure 6). Her recovery progressed well, allowing her to be transferred out of the intensive care unit after one week. She was then moved to the pulmonary department for continued management of her hydatid cyst.
DISCUSSION
Bronchoscopy is a commonly utilized diagnostic and therapeutic procedure, generally regarded as safe with a low risk of complications. However, rare and unexpected adverse events can arise, creating diagnostic and management challenges. Among these, the simultaneous occurrence of pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum after bronchoscopy is extremely uncommon, with only a few reported cases in the literature. This case underscores the importance of identifying such rare complications and understanding their underlying mechanisms to ensure optimal patient management.
The presence of free air in multiple anatomical compartments following bronchoscopy raises questions about the underlying pathophysiology. One widely accepted explanation is the Macklin effect [3], which describes alveolar rupture due to increased intra-alveolar pressure, leading to air dissecting along peribronchovascular sheaths and spreading to the mediastinum [4]. From there, air can further track along anatomical pathways to the retroperitoneal and peritoneal spaces.
Alternative mechanisms include direct air migration through fascial planes from the retroperitoneum, particularly in cases of high intra-abdominal pressure, diaphragmatic weaknesses, such as the foramina of Morgagni and Bochdalek, which may allow air to pass between the thoracic and abdominal cavities, or Microperforations or transient mucosal breaches in the airway or esophagus, which may not be evident during endoscopic reevaluation.
Pneumorrhachis (air within the spinal canal) and pneumothorax (air in the pleural space) are additional potential findings in such cases, though they were not present in our patient [5].
While pneumomediastinum is a known but rare complication of bronchoscopy, its association with pneumoperitoneum and pneumoretroperitoneum remains poorly understood and requires further investigation (Figure 4).
The nonspecific clinical presentation of these complications, ranging from mild discomfort to hemodynamic instability, can complicate early recognition. In this case, the patient initially exhibited abdominal distension, diffuse pain, and respiratory distress, which could mimic conditions such as gastrointestinal perforation, esophageal rupture, or peritonitis.
Given the lack of clear endoscopic evidence of perforation, imaging played a central role in diagnosis.
Computed tomography (CT) scanning remains the gold standard for evaluating post-bronchoscopic complications, allowing precise localization of free air and excluding life-threatening conditions requiring surgical intervention. In our case, imaging findings were critical in guiding further management decisions.
Literature reports indicate that pneumomediastinum often develops following medical interventions. For instance, Marwan et al. described a case where pneumomediastinum, pneumoperitoneum, and pneumoretroperitoneum occurred after colonic perforation during a diagnostic colonoscopy [6]. Similarly, Elkholy et al. reported a case in which accidental tracheal tube misplacement resulted in a dual presentation of pneumomediastinum and pneumoperitoneum [7]. These cases emphasize the importance of thoroughly assessing potential hollow viscus injuries, as a history of prior surgery may suggest iatrogenic causes.
The management of pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum (Figure 6) depends on the clinical presentation. In the absence of peritonitis, hemodynamic instability, or evidence of perforation, a conservative approach with close monitoring is often preferred. This underscores the diagnostic strategy proposed by Wang et al., which offers a structured framework for assessing cases in which air distribution serves as the main clinical indicator [8].
However, given the large pneumoperitoneum and associated clinical signs, surgical exploration was warranted in this case. The use of a minimally invasive laparoscopic approach combined with bronchoscopic reevaluation allowed for a thorough assessment while minimizing patient morbidity [9].
CONCLUSION
This case adds valuable insight to the growing body of knowledge surrounding rare post-bronchoscopic complications, particularly the triad of pneumomediastinum, pneumoperitoneum, and pneumoretroperitoneum. Although these conditions are uncommon, they should be considered in patients presenting with abdominal or respiratory symptoms following bronchoscopic procedures. The diagnostic challenges they pose are significant, but advanced imaging plays a critical role in accurately identifying these complications and guiding clinical decision-making. A multidisciplinary approach led to a timely and precise diagnosis, enabling the use of minimally invasive surgical management. This case underscores the need for further research to refine diagnostic algorithms and management strategies for such rare and complex presentations.
REFERENCE
1.
Vuong RQ, Liechty ST, Nicoara MD. Emphysematous changes in pneumoperitoneum and tension pneumothorax following robot-assisted bronchoscopy: A case report. J Surg Case Rep 2024;2024(1):rjad732. [CrossRef]
[Pubmed]

2.
Touati MD, Khefacha F, Ben Othmane MR, Belhadj A, Saidani A, Chebbi F. Fortuitous detection of adult malrotated ectopic kidney during acute appendicitis: A unique case report. Int J Surg Case Rep 2024;118:109679. [CrossRef]
[Pubmed]

3.
Wintermark M, Schnyder P. The Macklin effect: A frequent etiology for pneumomediastinum in severe blunt chest trauma. Chest 2001;120(2):543–7. [CrossRef]
[Pubmed]

4.
Chidambaram A. Revealing the Macklin effect: A unique case of spontaneous pneumomediastinum with subcutaneous emphysema. Chest 2024;166(4):A3558–9. [CrossRef]

5.
Dirie AMH, Aydın N, Hussein AM, Osman AA, Ahmed AA. Spontaneous pneumorrhachis, pneumomediastinum, pneumopericardium, and subcutaneous emphysema. Rare features of Hamman Syndrome. Ann Med Surg (Lond) 2022;74:103346. [CrossRef]
[Pubmed]

6.
Marwan K, Farmer KC, Varley C, Chapple KS. Pneumothorax, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum and subcutaneous emphysema following diagnostic colonoscopy. Ann R Coll Surg Engl 2007;89(5):W20–1. [CrossRef]
[Pubmed]

7.
Elkholy KO, Akhtar H, Landa E, Malyshev Y, Sahni S. A case of pneumomediastinum and pneumoperitoneum with concurrent massive subcutaneous emphysema due to repositioning of a tracheostomy tube. Cureus 2019;11(1):e3881. [CrossRef]
[Pubmed]

8.
9.
Hafiani H, Bouknani N, Choukri EM, Saibari RC, Rami A. Pneumoperitoneum, pneumoretroperitoneum and pneumomediastinum: Rare complications of perforation peritonitis: A case report. J Med Case Rep 2024;18(1):187. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Amrani Chaimae - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Bennani Samia - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Charif Saibari Rayhana - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Assakali-Rguig Anass - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Chirwa Abdillahi Mahamoud - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abdoulrazak Egueh Nour - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ayouche Othman - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rami Amal - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Amrani Chaimae et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.