|
Case Report
Moebius syndrome: A case report from Indonesia
1 Neurologist, Bhayangkara Raden Said Sukanto Hospital, Jakarta, Indonesia
2 Medical Doctor, Faculty of Health and Medicine, Atma Jaya Catholic University, Jakarta, Indonesia
Address correspondence to:
Maula N Gaharu
Email: mgaharu@yahoo.com,
Message to Corresponding Author
Article ID: 100107Z06MG2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Gaharu MN, Frederickson S, Natalia M. Moebius syndrome: A case report from Indonesia. Case Rep Int 2022;11:100107Z06MG2022.ABSTRACT
Introduction: Moebius syndrome is a neurological condition characterized by congenital facial uniplegia or diplegia due to peripheral type facial nerve paresis and lateral eye movement paresis due to abducens nerve paresis resulting in strabismus. Incidence of Moebius syndrome is 0.27/100,000 live births and often associated with abortion attempts. The following is a case report of Moebius syndrome in Indonesia of a 14-year-old girl with a history of attempted abortion by her mother.
Case Report: A 14-year-old girl came with facial muscle complaints in the form of difficulty in raising both eyebrows and closing the mouth since birth. These complaints cause difficulty in eating and drinking. Complaints accompanied by abnormality of the limbs and the number of finger in toes and hands. The patient’s mother had a history of attempted abortion by taking the chemical disinfectant chloroxylenol 4.8% and other drugs. There was bilateral facial nerve paresis and cognitive impairment. On examination of brain magnetic resonance imaging (MRI), it was within normal limits. The patient was planned for physiotherapy and consulted to orthopedics.
Conclusion: Moebius syndrome is a collection of rare neurological clinical manifestations in children. Exposure to chemicals during pregnancy can be the etiology of this syndrome in addition to genetics. Management of Moebius syndrome is limited to supportive and symptomatic approach.
Keywords: Chloroxylenol, Cognitive impairment, Facial nerve, Moebius syndrome
INTRODUCTION
Moebius syndrome is a neurological condition characterized by congenital facial uniplegia or diplegia due to peripheral type facial nerve (Nervus VII) paresis and lateral eye movement paresis due to abducens nerve paresis (Nervus VI) resulting in strabismus [1]. Moebius syndrome can also involve other cranial nerves with deformities and other various manifestations of congenital malformations belonging to the large group of oromandibular-limb hypogenesis syndrome (OMLH) [2]. The incidence of Moebius syndrome is 0.27/100,000 live births and is often associated with abortion attempts [3]. It is a rare neurological condition that has received little attention in clinical diagnosis and so its incidence is not widely reported in daily practice. The following is a case report of Moebius syndrome in Indonesia of a 14-year-old girl with a history of attempted abortion by her mother.
CASE REPORT
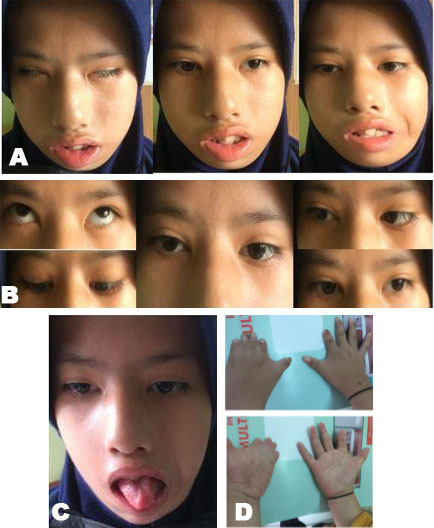
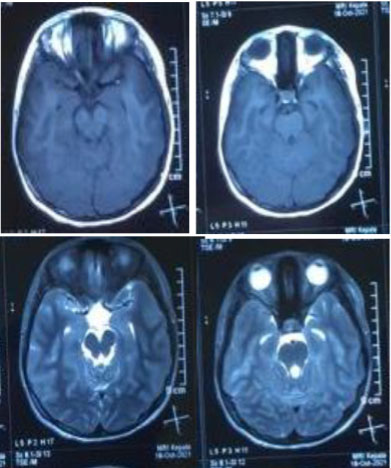
A 14-year-old girl came with facial muscle complaints in the form of difficulty in raising both eyebrows and closing the mouth since birth. These complaints cause difficulty in eating and drinking. Complaints accompanied by abnormality of the limbs and the number of finger in toes and hands (Figure 1). The patient also has an inability to go to school as usual because it is difficult to follow school lessons. The patient was born at term. The patient’s mother had a history of attempted abortion by taking the chemical disinfectant chloroxylenol 4.8% and other drugs. On general examination, hemodynamics were within normal limits, local status showed syndactyly. On neurological examination, there was bilateral facial nerve paresis and cognitive impairment. On examination of brain magnetic resonance imaging (MRI), it was within normal limits (Figure 2). The patient was planned for physiotherapy and consulted to orthopedics.
DISCUSSION
Moebius syndrome is one of the rare congenital diseases characterized by unilateral or bilateral non-progressive paresis of the facial nerve (Nervus VII) with impaired ocular abduction due to disorders of the abducens nerve (Nervus VI) [4]. In 1888, the German neurologist Paul Julius Moebius first described the clinical manifestations of Moebius syndrome, namely, paralysis of the facial and abducens nerves. However, it was von Graefe who first reported weakness in the facial muscles [5]. Moebius syndrome may also be accompanied by paralysis of other cranial nerves such as the oculomotor (III), trigeminal (V), vestibulocochlear (VIII), glossopharyngeal (IX), vagus (X), and hypoglossal (XII) nerves; orofacial disorders, behavioral and cognitive disorders, orthopedic defects such as syndactyly, brachydactyly, or adactyly. The prevalence of Moebius syndrome is about 1 in 250,000 births with the same incidence between men and women [4]. Chowdhury et al. reported the incidence of 2–20 cases per 1 million births, although sporadic, Odoardo et al. reported cases in the family found in 2% of cases [1]. Towfighi et al. classified this syndrome into four groups based on pathological differences, namely hypoplasia or atrophy of the cranial nerve nuclei, primary lesions of the peripheral cranial nerves, focal necrosis of brainstem nuclei, and primary myopathy without central nervous system (CNS) or cranial nerve lesions [6].
The causes and pathogenesis of Moebius syndrome are unclear and controversial. Since the first time Moebius syndrome was introduced by von Graefe and Moebius, there have been various debates about whether Moebius syndrome is caused by genetics or not, but it is thought to be related to environmental and genetic factors. Although the associated gene has not been identified, it is thought to be associated with changes in specific regions of chromosomes 3, 10, or 13. Use of certain drugs can be a risk factor. In addition, the possible causes of Moebius syndrome are exposed to toxic substances, impaired rhombencephalic vascular development, and ischemic or hypoxic events after the fifth week of gestation [4]. Misoprostol is one of the substances that is often reported to cause Moebius syndrome. It is a synthetic analogue of prostaglandin E1 which has greater anti-secretory and mucosal protective activity than prostaglandins, usually used to prevent and treat gastrointestinal lesions caused by non-steroidal anti-inflammatory drugs (NSAIDs) and upper gastrointestinal ulceration [7]. The use of misoprostol is not recommended during pregnancy because it can stimulate contractions of the uterus and cause vaginal bleeding so that it can endanger the safety of the fetus [7]. The combination of misoprostol and mifepristone or methotrexate are often used for elective induction of abortion [7]. In this patient, her mother had a history of taking chloroxylenol 4.8% and taking other drugs for abortion. The authors did not find literature discussing the relationship between consumption of chloroxylenol with Moebius syndrome. In many cases, chloroxylenol consumption causes intoxication related to the need for treatment due to effects and complications such as decreased consciousness, cardiac arrest, bronchospasm, respiratory distress, laryngeal edema, upper respiratory tract obstruction, and gastrointestinal bleeding [8]. This can be attributed to hypoxic ischemic events as one of the suspected etiologies of Moebius syndrome [1]. However, the relationship between consumption of chloroxylenol and Moebius syndrome needs to be studied further.
Lineu et al. reported 90% of cases with clinical manifestations of bilateral facial nerve paresis of central or peripheral type. It is a clinical condition that is often found soon after birth, in the form of eyes not closing completely during sleep and difficulty sucking while breastfeeding. However, in some cases, this clinical manifestations are not seen for several weeks or months, until it is only visible when the baby smiles and through facial muscle movements. Other cranial nerve deficits may also occur, with 50% of cases are hypoglossal nerve paresis. Other manifestations in the form of brachial malformations, especially in the upper extremities and 30% of cases occur bilaterally, in the form of congenital amputation, clubhand/clubfoot, syndactyly, and brachydactyly. Cognitive disorders such as autism and mental retardation may also occur. In this patient, facial nerve paresis was marked at birth, the patient was unable to breastfeed and had to be assisted with a spoon. Brachial malformations were also found in both extremities bilaterally and with moderate cognitive impairment.
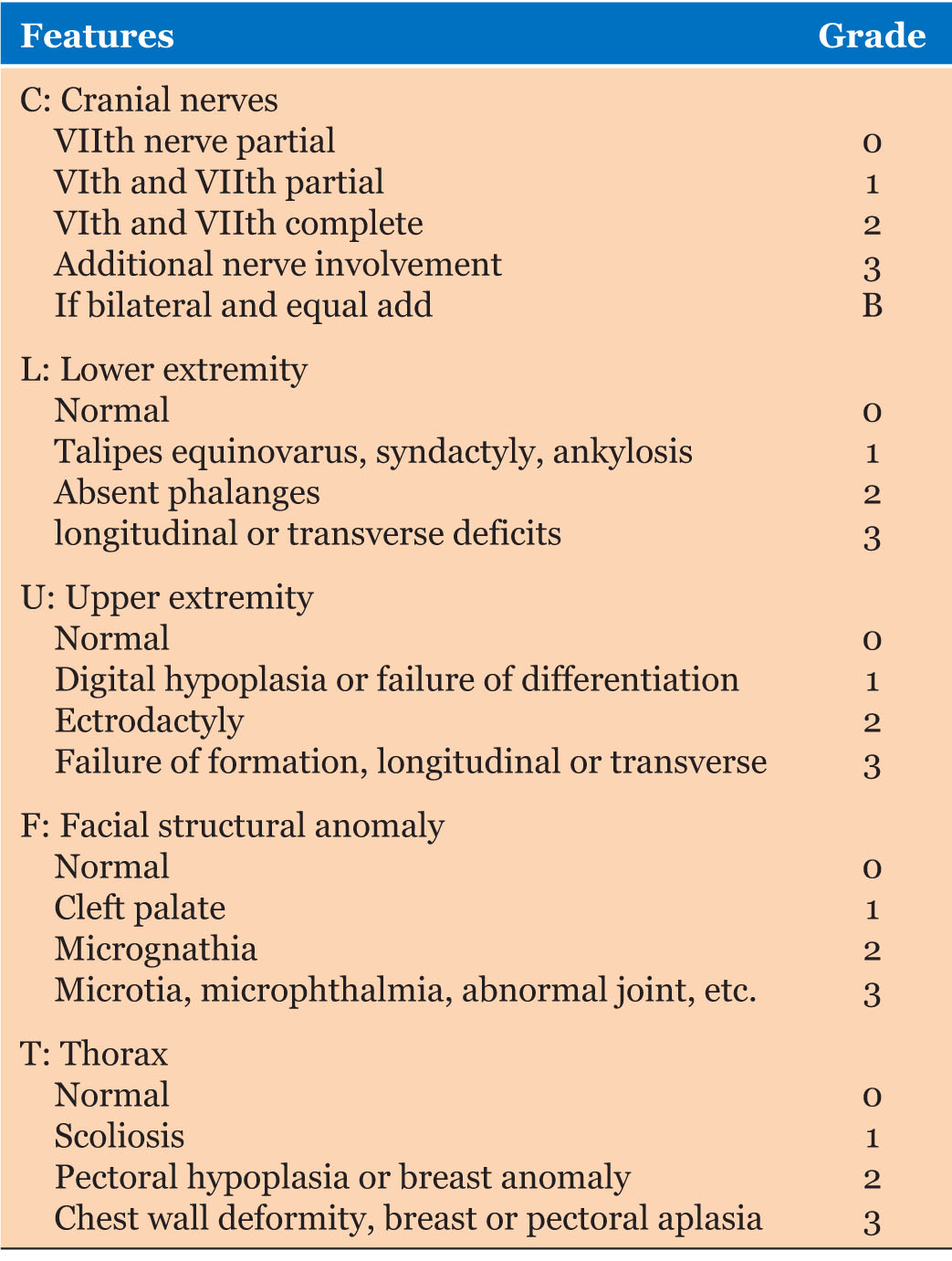
The diagnosis of Moebius syndrome was made based on clinical criteria [9]. There are no specific laboratory tests associated with this syndrome [5]. Radiological imaging is less helpful in establishing the diagnosis. Head computed tomography (CT) scan occasionally reveals calcification of the site of dorsal ischemic necrosis of the pons. A magnetic resonance imaging (MRI) of the head may reveal brainstem hypoplasia. Abramson et al. (1998) proposed the CLUFT scoring system (Cranial Nerves, Lower extremity, Upper extremity, Facial structural anomalies, Thorax) [5],[9] (Table 1). Classification and assessment of the degree of dysmorphic disorder has several functions. First, to categorize the degree of anomaly by location and severity. Second, it is possible to compare different patient groups and analyze the surgical management. Finally, systematic study of the spectrum of disorders can provide insight into the pathogenesis. In our case report, brain MRI is normal and the total score was 9B on CLUFT, which consists of bilateral facial nerve paresis variable peripheral type, partial abducens nerve paresis and hypoglossal nerve paresis (4B), absent phalanx in the lower extremities (2), digital hypoplasia or failure of differentiation (1), micrognathia (2), and the thorax tends to be normal (0).
CONCLUSION
Moebius syndrome is a collection of rare neurological clinical manifestations in children. Exposure to chemicals during pregnancy can be the etiology of this syndrome in addition to genetics. Definitive treatment is not yet available for Moebius syndrome. Therefore, management is limited to supportive and symptomatic approach. Parental education plays an important role in the patient’s life. Facial nerve palsy results in a mask-like face and an inability to smile. Restoration of movement due to the paralysis is the main goal of the treatment plan. Management includes reconstructive plastic surgery with muscle transplantation which is ideally performed at an early age. Ocular, orthognathic surgery and surgical correction of other associated abnormalities may be indicated. Other intervention programs such as physiotherapy for congenital orthopedic problems, occupational therapy to assist the patient’s activities of daily living, or speech therapy for patients with severe facial nerve palsy may be supportive. Eyes also need to be considered to avoid exposure to keratitis, ulceration, and corneal abrasion.
REFERENCE
1.
Chowdhury S, Sarkar S, Guha D, Dasgupta MK. Moebius syndrome: A rare entity or a missed diagnosis? J Pediatr Neurosci 2020;15(2):128–31. [CrossRef]
[Pubmed]

2.
Pedersen LK, Maimburg RD, Hertz JM, et al. Moebius sequence – A multidisciplinary clinical approach. Orphanet J Rare Dis 2017;12(1):4. [CrossRef]
[Pubmed]

3.
Carta A, Favilla S, Calzetti G, et al. The epidemiology of Moebius syndrome in Italy. Orphanet J Rare Dis 2021;16(1):162. [CrossRef]
[Pubmed]

4.
Picciolini O, Porro M, Cattaneo E, et al. Moebius syndrome: Clinical features, diagnosis, management and early intervention. Ital J Pediatr 2016;42(1):56. [CrossRef]
[Pubmed]

5.
Ghosh R, Shetty V, Hegde S, et al. Rare features associated with Mobius syndrome: Report of two cases. J Dent Res Dent Clin Dent Prospects 2017;11(1):60–5. [CrossRef]
[Pubmed]

6.
Towfighi J, Marks K, Palmer E, Vannucci R. Möbius syndrome. Neuropathologic observations. Acta Neuropathol 1979;48(1):11–7. [CrossRef]
[Pubmed]

7.
Pastuszak AL, Schüler L, Speck-Martins CE, et al. Use of misoprostol during pregnancy and Möbius’ syndrome in infants. N Engl J Med 1998;338(26):1881–5. [CrossRef]
[Pubmed]

8.
9.
Abramson DL, Cohen MM Jr, Mulliken JB. Möbius syndrome: Classification and grading system. Plast Reconstr Surg 1998;102(4):961–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
We are grateful to our patient.
Author ContributionsMaula N Gaharu - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sandy Frederickson - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Maria Natalia - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Maula N Gaharu et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.